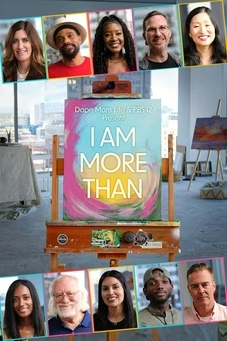
Decode Colorado
Decode: Social Determinants of Health
Special | 29m 59sVideo has Closed Captions
Decode Colorado, digs into the healthcare landscape in Colorado.
When you consider how, when, and why you get sick or deal with certain health conditions, are factors like race, socioeconomic status, and environment taken into consideration? If not, the impact might be surprising. The latest episode in the Heartland Emmy award-winning series, Decode Colorado, digs into the health care landscape in Colorado to understand the social determinants of health.
Problems playing video? | Closed Captioning Feedback
Problems playing video? | Closed Captioning Feedback
Decode Colorado is a local public television program presented by PBS12
Decode Colorado
Decode: Social Determinants of Health
Special | 29m 59sVideo has Closed Captions
When you consider how, when, and why you get sick or deal with certain health conditions, are factors like race, socioeconomic status, and environment taken into consideration? If not, the impact might be surprising. The latest episode in the Heartland Emmy award-winning series, Decode Colorado, digs into the health care landscape in Colorado to understand the social determinants of health.
Problems playing video? | Closed Captioning Feedback
How to Watch Decode Colorado
Decode Colorado is available to stream on pbs.org and the free PBS App, available on iPhone, Apple TV, Android TV, Android smartphones, Amazon Fire TV, Amazon Fire Tablet, Roku, Samsung Smart TV, and Vizio.
- Major corporate support for decode Colorado social determinants of health was provided by Intermountain Health and made possible by viewers like you.
- In the United States, Healthcare is not a right, it's a privilege.
And in most of the world, Healthcare is a right.
And health care the way we think of it, go to the doctor, go to the hospital.
It's just a tiny fragment of really a broader picture of health.
- There's social determinants of health, like housing and security, food insecurity that preclude access to healthcare, cause you're not going to be worried about your diabetes when you can't get food for your kids.
- If you are accessing the healthcare system without financial means, that debt then is going to make it so that you are challenged to take care of other parts of your life, which can also impact your health.
- If you don't have transportation, if you don't have housing and you don't have food, that complicates your ability to be healthy and your ability to access care.
- As healthcare providers, we have an ethical responsibility to make sure that families have that access.
- As a doctor, if they need to understand them as a person, understand their social determinants of health as a whole person as part of a community as well.
- Families may feel that there's no solution to this problem.
There's just nothing we can do.
- Programs that sit outside of the conventional healthcare system, they're of critical importance.
- Through addressing social determinants of health needs, we're trying to reduce or mitigate the impact on your health.
- When you think about health care, some people just think I go to the doctor and I get a shot or I get a prescription.
But really, many of those treatments could be avoided if we thought more openly about what impacts our ability to lead a healthy life.
- Where you live has a lot to do with what your house is.
If your ZIP code is a higher income zip code, you have more sidewalks, you have more bike lanes, you have more parks, which impacts a family's abilities to take their kids outside safely.
- If you live in a community that has maybe lots of factories, there might be high incidence of asthma in that community.
- If you're surrounded by air pollution.
Or in more rural areas, it could be cow feeding farm.
There are effects on the health.
- If you have to take two buses to get to your healthcare provider, that becomes a barrier.
- If you can't get in a car and go to work, you can't work.
- If people don't have grocery stores, maybe they're not going to be able to eat as healthy.
- Those are all things that affect almost all communities in the United States right now, whether it's rural or urban, people have challenges with social determinants of health.
- Without a doubt, I think the greatest social determinant of health that we need to address in Colorado today is housing.
Access to housing.
Housing inventory, housing affordability, housing safety.
This is mission critical.
- I was here sleeping for almost 2 years.
Every night I would just grab some cardboard and make a little bed and sleep right here.
I had a lot of bad times where I couldn't sleep.
I was concerned that someone was going to walk by and try and steal my backpack because everything I own was in my backpack.
It was tough, for sure.
Growing up, it was pretty basic.
I found skateboarding as an outlet, running, golf, skiing when I was in my senior year of high school, I received a scholarship for skiing, which I unfortunately lost after falling during the state championship my senior year.
Like fractured my tibia.
I remember clipping that gate and immediately thinking it was a total downfall for me in my life.
I kind of kept to myself.
Music was really big with me.
My sister was an amazing musician.
The two of us kind of bonded on that.
That's probably my favorite photo my sister.
I knew that I was not going to ski again.
I had a lot of friends that were professional snowboarders, and they kept egging me on to give it a try.
And one of them just gave me a board one day.
That drive kind of kicked back in the same drive that I had when I was skiing.
I got to meet some very interesting people.
That's kind of how I got connected with getting sponsors.
I was a very social person and I was general manager of a very successful company.
I was competing.
I had my first TBI in Vail, overshot my landing and hit my shoulder and my head.
I woke up in the hospital.
So I don't remember anything, but I did have a seizure the next day.
My second TBI was about six months later.
I immediately lost 2 sponsors.
What spiralled me to homelessness was when I lost my sister.
She passed from breast cancer that metastasized to her liver, lungs, kidneys, hip, spine and brain.
Everything that I felt was me... Gone.
And I just shut everything out.
I would sleep a couple hours at best, then I would just be awake.
I couldn't shut my mind off.
The only thing that was resolved was alcohol, because it would just blank my mind.
- There are so many assumptions we make about people without understanding their context.
You can't divorce a human or a family from their context, and their context matters.
- I don't think most of us realize and until you're close to it, how close to homelessness any of us are.
If something went wrong, it could be me in a few months.
It could be most people within a few weeks or months or certainly years.
It's really important that we be able to have an address for an individual first that they have housing where they are safe from the cold or it's perhaps other influences in their life if they're living on the street.
If we don't have a way to contact those individuals and they're moving from place to place.
It just disrupts our ability to care for them.
- I hadn't taken my shoes off.
They were just soaking wet and freezing.
I was just ignoring the symptoms.
I woke up here one morning and just something clicked and I decided that I wasn't going to be staying here.
That evening that I needed a change, I knew that I'd have a better chance of finding a job downtown.
I hop the light rail, dodging security and made it all the way to Union Station.
And then I walked into the Starbucks and that's where I had my seizure and that's what brought me to Saint Joe's.
And that's where they found the bone infection in my toe.
- We screen all in patients for social determinants of health, and it's just another way of humanizing an aspect of a patient stay here when sometimes you know they're not really recognized for the human that they are.
And so we want to continue that mission of just doing our best to to make people feel valued.
To feel like we see them as a person.
We keep a vast supply of clothing for our homeless population, and so we've got T-shirts and sweaters and coats.
And so we keep it for a lot of our patients that do come in off the streets here in downtown Denver.
- We actually partner right now with the Colorado Coalition for the Homeless.
We lease 13 beds for our homeless population.
- We are partnered with all the main hospital systems in Colorado.
They basically reserve beds, so we have these annual contracts with them where they have a bed reservation kind of a guarantee that if someone meets criteria for the program.
They'll have a place to send someone at discharge.
- Case manager at Saint Josephs has set up the interview with Stout St. Recuperative Center, where I went after a surgery that I had because of frostbite.
I didn't like sitting in my room.
That's when I offered to help out with cleaning with the kitchen, with activities, anything I could.
I gave up alcohol and replaced that addiction with a new addiction which is communicating with people.
The program manager, Mariah, and my case manager invited me into the office one day and they asked if I'd be willing to accept a housing voucher because I was pre selected.
This is home.
This is where I live and I love it here.
I'm very grateful and thankful to be here.
- Housing is health and I think would be very easy in the clinical setting for there to be miscommunication, misunderstanding about the presenting symptom that the patient shows up with, and what's really going in their life that caused that.
- And the holistic view is not what you learned during residency.
It's like, how do you be efficient, fast, make these diagnosis and going about your business.
That wasn't what people needed.
They needed me to understand them as a person, understand all the challenges they were having, even to get to that clinic.
- I am a native of Denver.
I've been here all of my life.
We had a cosmetology lab in our high school.
I really enjoy the art of beauty and the art of makeup, and in 1979 I opened my salon.
So it's been a dream come true, something that I wanted to do.
Most people come every two or three weeks.
I come every week because I need therapy.
- Good morning.
I'm here on behalf of the call of the Black Health Cooperative because we have a blood pressure screening program that we run in salons and Barber shops throughout Denver and Aurora.
So what I've tried to tell people is take a few deep breaths and let it out.
It's a great space.
It's a trusted space.
People come in very regularly.
They probably go to see their hairdresser way more time than they go to see their doctor and they feel comfortable here.
They feel at home and you look at this shop, you really feel relaxed and at home you've got people that you know and trust.
- Alright, darling.
- Walls, the owner of this shop, has been around over 40 years.
It's been such a stigma in our community about doctors and being afraid to even go to a doctor.
People know that we're stable and that they can always look forward to come here and not only get a good hair do, but to have their blood pressure taken.
So it's been a blessing.
- That goes to the very sacred space that people are in when they're with their healthcare providers.
You have to be able to be vulnerable.
You are in a very vulnerable place to talk about your health and the realities of your life that may make it difficult to just follow the care plan that your doctor says is necessary to take care of yourself.
- We learned in the pandemic [INDISCERNIBLE] wide just how acute the gaps are particularly for communities of color in our healthcare system today.
- Going in to see a provider is part of the equation of being healthy, but still people don't necessarily trust the health systems and not to just go to anyone.
And the people that are coming to me, they said I have nothing against anyone else.
I just want someone with lived experience.
That's why when people say well we don't need to know about the history, you need to go back because the foundations of why the black experience is so different.
Lies in the history of how we got here, and it's still unfortunately playing into how we were treated in America.
We have a long and unfortunate history of experimentation on certain populations.
- The men had no idea they were being used as Guinea pigs in an experiment designed to follow them to their deaths.
- When you think about Tuskegee, that the public health institution thought it was OK to take these illiterate men and not treat them for disease, even when the treatment was available.
But multiple surgeries on black women without anesthesia, women were sterilized, and a lot of times the women didn't know.
So it wasn't voluntary.
- They sterilize me.
What do you think I'm not worthy?
We've got many unintentional negative impacts happening today that serve to just compound the remnants of the intentional systems that were built and never fully dismantled.
- So I think it's not unusual for people to say, well, I'm not sure I trust that dctor, it may be a distrust of the whole medical profession.
When I go places, I don't introduce myself as a doctor because I want to see how people are going to treat me, by going If I'm a doctor, ohh all of a sudden, you know, people can do different things.
But if I just go in with my black woman self, then sometimes I'll not treat you so well even in the healthcare system.
- Now I think we can do a better job.
It's not for lack of resources.
We're spending more money that has ever been spent in the history of the world on healthcare, and yet the results aren't good enough.
It's part of the relational piece, You really have to trust me to share all of those details.
And then if we can talk about it a little more, there are other things that we may be able to address.
- Sometimes, even when they don't get their blood pressure checked, we were talking about other things that are important in their lives.
And so I like hearing about peoples lives.
I mean, that really is what shapes who they are.
- Well, I tell you, if it had not been for those screenings that were coming in, I don't think I would be here today.
[INDISCERNIBLE] She takes care of business and she was going to the doctor regularly.
And so she's a real champion here.
She always tells people to come over and get their blood pressure checked.
So she said, "Oh yeah, I'm going to show you guys.
It's easy."
So she came over, she got her blood pressure checked and it was high.
- Not only did I have high blood pressure, but my kidneys were having some struggles and so I had to go through treatments for my kidneys.
And had I not done this little simple sitting there for 3 minutes to get my blood pressure taken, I could have lost my life.
- After that, she became quite a champion.
She's like, this is great staff.
They're meeting people where they are.
They're not trying to take over for the doctors, but they're here to support.
- It's certainly easier to get your blood pressure taken if you're going to be there anyway.
But if you have to go somewhere to get your blood pressure taken and go somewhere to get your bone density checked or go somewhere to get your heart rate checked, it may be easier to just "I'll do that next week".
So of course one of the newer innovations is telehealth.
It fits the bill for a lot of things if you are homebound.
If transportation is an issue.
If you can't take off from work, but you got a 15 minute break, it makes the rest of your life easier.
- We have the capability and capacity through technology and data and data science to care for the entire spectrum of illness, from the sickest of the sick for patients in rural hospitals, in the ICU to patients who are at home with chronic or complex medical conditions where we can surveil to look for patients who are deteriorating before they're symptomatic and then we can intervene before they even know that they're sick and prevent hospitalizations, prevent illness, prevent death.
At any given time, we're monitoring thousands of patients.
- Hey, this is Doctor Davis from UC health.
Yeah, tell me how you're feeling?
- And I like to say as hard as COVID was, there are a number of silver linings and virtual health was one that does great things for both the patient and for the provider.
The main aspect is one of those social determinants of health transportation.
We eliminate that as being an issue, and so I think it's a great innovation for all of the healthcare systems in the US.
But I think there's a place for virtual care, and there's a place for face to face.
Some people are uncomfortable with technology, may distrust technology and think that you know who else can see this.
- And then there's the digital divide.
There are people in urban areas and rural areas who are not going to be able to access the technologies or equipment they need.
- One of the things we learned in surveying some of the rural areas is that there's still this struggle with broadband.
So that can make it much more challenging.
I think the flip side of that is there is this community feel.
There may be local organizations or churches who are much more connected to the entire community than we would have in an urban area.
- Access to healthcare and rule setting is a social determinant because it's the context in which they have to live.
- I was pregnant with twins.
The plan was to make it to 37 weeks pregnant, which is full gestation for twins.
And then in Ray, Colorado, which is about an hour and a half away, we were going to have a delivery there.
A planned delivery.
They decided to make a little bit of an early debut, so we found ourselves in a bit of an emergency here in Cedric.
The closest major city is about 3 hours away.
- I was notified that they have a preterm labor situation, with one going to be a breach delivery.
- And just several months prior, we had dismantled our OB department and I'm used to, "let's go to this room.
"We can get this card and get the supplies."
While that was no more and big part of that is just all the education you need.
All the nurses need to be trained in the unnatural the resuscitation.
Then you have to have anesthesia available 24/7.
With routinely for years delivered on 20-25 infants a year, and that had fallen off to like 10, and it just didn't seem to be practical anymore.
- We're constantly evaluating the revenue cycle for where can we get more efficient?
Where can we maybe eliminate something that's you know not necessary or takes up too much time.
So it's a strain, but it's one that we understand as part of our current operating condition and are just constantly looking for ways to improve.
- In general, you have such a paucity of resources in rural areas compared to urban areas, so any new development technology offering that the healthcare system might develop, it's going to pose a lot of barriers to getting resources in a rural setting.
- The resources aren't there to provide acute hospital care in every single one of our 64 counties, but we try to stitch together a system of collaboration to deal with that.
- As Doctor Dyer was reaching out to Nikki, was, they said do not have these babies until we get there basically.
- They came from Colorado Springs.
So we had to wait four and a half, five hours.
- So they headed this way.
They actually had two incubators, but a team can only take one patient.
They actually recruited another team who then flew to Ogallala and our ambulance picked them up.
Now we had two teams of neonatal specialists that could handle both babies.
- The best thing to do is to have a C-section at that point.
And I was like [BREATH] - As it turned out, as we were delivering, the second team arrived.
- When both twins were delivered, she was first and we heard her cry.
So that was, I mean, It was emotional.
And then a minute later comes Henry and he screams too.
They literally ran them into the other room to start working on them.
- Before they left, they wheeled my bed out to the hallway so that I could see them and their little pods before they got transported.
- He was kind of struggling a little bit, so apparently somewhere down the line they were able to get a helicopter to brush.
They took him up.
- The EMT crew transported me up there, and Cody followed behind us and I just remember them getting me off the ambulance and Kaylin was just like " are you eady to go to see those babies?"
And I lost it.
- I think some of the most exciting innovations are not necessarily connected to technology and more connected to what we can do in models of care.
Those kinds of models where we can think about what are the needs of people that may go beyond healthcare, but absolutely impact their health and Wellness and for us to work in partnership with Community resources, that's going to make the real difference in what we can do in healthcare.
[SPEAKING IN SPANISH] - I love to just see the world through their eyes, you know?
They're just so creative and adventurous and outgoing and just ready to learn.
[SPEAKING IN SPANISH] When you become a mom in my culture, it's just like, oh, you just take on it and you just go with it.
And I'm just like, how do you just go with it?
What is there more to motherhood?
As, like as an individual?
Like, what is me?
Who am I?
That's what is one of the things that still was trying to find that piece were like that.
I'm not just a mom that I'm also like a woman who also has goals, who also has dreams.
You know, how can I say, listen to that side of me.
I became pregnant when I was 20.
Because I was in college, I was still trying to get my degree.
My husband, he's also a business owner and he's like he was gone and I'm home during the pandemic and I'm dealing with the kids.
It was hard at the beginning to be like, OK, maybe we do need help with food.
Cause having to kids at home and it was like milk runs out really easily.
You know when you start noticing things like that bread just essentials.
I was like hey, well, how can I help my family?
That's when someone told me about Resource Connect.
Alright, good.
Open it.
Open it.
Open it.
- The process for a family that's referred to Resource Connect starts in the clinic itself.
There's a Screener that's provided, and depending on what they mark on that cycle social screener, then they're connected to a community health navigator.
- Who wants to go frist?
- A lot of families tend to feel more comfortable sharing their situation, when they don't feel like, oh, they're just going to judge us or ask us more questions or things like that.
It makes a difference.
[SPEAKING IN SPANISH] - One of our roles as pediatricians is really to think about lifelong health of the child and what can I do to impact their health trajectory.
We know one of the most important determinants of lifelong health is your income.
And I can't Provide comprehensive care, if I'm not addressing the situation that's at home and how their income status might be affecting them.
- They guide us through the whole process, so when we go to their appointments, they ask me like, what do you need help?
We fill out the survey.
I would ask them about any classes that I could take.
They have children's museum visit and the food pantry.
- As healthcare providers, we really need to make the link between nutrition and health, so it comes with education.
It comes with the recipes it comes with, all sorts of fun things about how to get your kids to eat fruits and vegetables.
Everything we do here is philanthropy funded, so we really have a great relationship with our donors.
You know, they really understand what we're trying to do here and they understand that it's all for the kids.
It's for the families.
And we really do want to keep kids out of the hospital.
- How do we address social determinants of health?
How do we look at healthcare in a more holistic way?
Look at the entire person, the entire family unit understand the reality of their lives so that we're not treating this little sliver that can be discussed in a clinic setting.
- I would like for us all as a country to resist our urge to judge, because I bet you most time we have made some completely wrong assumptions.
If we just took a moment to ask rather than judge, we would completely shift the human dynamic in this country.
- I am optimistic.
I think there's a lot of excitement around where Colorado's headed think people are getting tired of looking around and seeing despair and the way you prevent despair is connection and that's how we all get it, invest and fix this together.
- I think that the people that are making decisions for our hospital and our hospital system have healthcare at their very heart and soul, and I have faith that they'll make the right decisions and we just have to be strong and be optimistic and be faithful that everything will just keep going forward.
- There we gotcha.
- At the end of the day, I think medicine succeeds because it's relationship based.
It's about building partnerships and relationships with trusted people to be able to care for the populations that we need to take care of.
Decode: Social Determinants of Health
Preview: Special | 29s | Decode Colorado, digs into the healthcare landscape in Colorado. (29s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorshipSupport for PBS provided by:
Decode Colorado is a local public television program presented by PBS12